A weak pancreas needs to follow a diet, especially during periods of exacerbation of pancreatitis and other chronic diseases of this organ. We will present the menu for the pancreas for the week in this article. But before starting a diet, you should understand why, with an exacerbation of pancreatic disease, you urgently need to change your diet.
Menu for the pancreas for the week
Diet for diseases of the pancreas: main stages
It should immediately be noted that the diet at different stages of the development of the disease varies greatly. So, with a sharp exacerbation of pancreatitis, everything except mineral still water (1.5 liters) should be completely excluded from the pancreatic patient’s diet in the first two or three days. You should drink water in small portions (no more than 200 ml). In addition to mineral water, it is permissible to drink up to two glasses of rosehip infusion. This approach will prevent further deterioration of the pancreas, symptoms of the disease and diet will reduce the production of stomach enzymes.
After the first three days at the acute stage of the disease, the menu can be diversified. During the week, it is better if the diet is low-calorie, from which fats and carbohydrates should be excluded as much as possible. Meals must be divided (at least five meals a day). All dishes must be steamed or boiled and have a liquid or mushy consistency.
At this stage, the main task of the menu is aimed at protecting the stomach and preventing the disease from becoming chronic.
After the main symptoms of the disease subside and it goes into remission, you can experiment with the menu. The diet should be varied, as other healthy organs need it. Therefore, you can increase your consumption of vegetables and fruits, in addition to sour ones and those rich in coarse fiber. It is better to give up fatty meats, anything fried, alcohol, and baked goods.
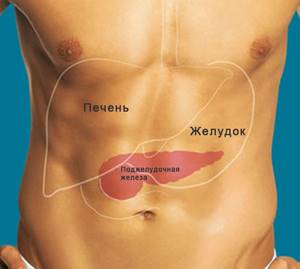
In chronic cases, the diet for liver and pancreas disease is aimed at preventing exacerbations. It comes down to fractional meals with the rejection of carbohydrates that are quickly digestible for the stomach, as well as everything fried, spicy and sour. It is necessary to drink plenty of water (at least 1.5 liters per day). Otherwise, the diet for chronic diseases of the stomach and pancreas is not much different from normal nutrition.
Diet during exacerbation
Diet violations or adverse effects, stress contribute to the fact that inflammation of the pancreas enters the acute phase. In addition to severe painful attacks, the patient is bothered by nausea, vomiting, and sometimes diarrhea. The patient suddenly loses weight.
It lasts from two to five days. Food is prohibited, the patient is allowed to drink one glass of warm still water every hour.
At the end of the fast, slowly and carefully, observing the patient’s well-being, he is given small portions of ground porridge and vegetable soups. Meals at short intervals, 6–8 times a day. It is important to feed only fresh foods that are prepared immediately before consumption. Alternate cereals and vegetables. The basis is a set of recommended products from the therapeutic diet, table No. 5.
General principles of diet
Despite some differences in the menu of a sick person at different stages of development of diseases of the stomach and pancreas, they are all aimed at achieving one common goal - complete recovery of the body or, at least, preventing serious complications of the disease. Therefore, in case of pancreatic disease, nutrition and diet have several general principles.
Fractional nutrition for the pancreas
Basic principles of diet for pancreatic disease:
- fragmentation of therapeutic nutrition: food should be taken in small portions 6 times a day to avoid stress on the walls of the diseased stomach;
- grinding the food consumed: when the pancreas is diseased, the organ responsible for digesting food suffers, so for recovery it is necessary to reduce the load on the stomach;
- avoidance of foods rich in fiber, as they stimulate the production of enzymes;
- reducing the amount of fats and carbohydrates in the diet, because their absorption puts additional stress on the diseased organ;
- refusal of animal proteins in favor of plant proteins, which are more easily broken down by the gastric mucosa;
- taking a large amount of water, since during the recovery period the body consumes a lot of fluid, and there is a risk of dehydration.
Nutrition for pancreatitis in adults

The diet for pancreatitis, which the doctor prescribes, is based on the principles of proper nutrition. Patients are advised to eat small meals 5 times a day. You will have to eliminate unhealthy foods from your diet forever. For diseases of the pancreas, it is necessary to eat mainly protein foods, and it is better to reduce the consumption of fats and carbohydrates to a minimum. Following a diet without disruption is possible by drawing up a menu for the week ahead. When compiling your diet, consider the following recommendations:
- do not skip meals (eat every 3-4 hours);
- eat in portions of 150 g;
- grind food if it can irritate the mucous membranes;
- It is better to choose dishes with a high protein content;
- forget about excessive consumption of fats and carbohydrates forever;
- refuse dishes with a high content of extracts;
- In case of severe pain, refuse food for two days.
It is much more difficult for those with a sweet tooth to maintain such a diet, because they cannot eat their favorite sweets, cakes and cookies.
Products that are allowed for pancreatic disease
The list of foods that can be eaten by people with a diseased pancreas includes:
Diet soup
- vegetable soups, with the exception of those to which white cabbage is added;
- porridge (oatmeal, rice, pearl barley, buckwheat);
- lean meats and poultry (veal, chicken, etc.);
- any types of snacks in the form of salads (suitable from both raw and boiled vegetables);
- low-fat fish;
- baked goods are also allowed, but it is better to consume them in a dried state, or one day after baking;
- eggs are allowed in small quantities and only soft-boiled or steamed omelet;
- dairy products such as kefir, cottage cheese, sour cream for dressing (it is better to choose one with a low fat content);
- fats are allowed only in oil (butter or vegetable);
- vegetables (pumpkin, green peas, potatoes, tomatoes, cucumbers, beets, carrots, etc.);
- pasta made from premium flour;
- berries (except for sour ones);
- drinks in the form of non-acidic fruit juices, tea with milk, rosehip tincture, compote, jelly.
Products prohibited for pancreatic diseases
For people suffering from acute or chronic forms of pancreatic disease, there are quite strict restrictions on the consumption of certain products.
These include the following:
This food is contraindicated for consumption in gastrointestinal diseases.
- fatty fish;
- rich broths, as well as soups in the form of cabbage soup and borscht, as they are sour and irritate the gastric mucosa;
- flour products in the form of rye bread or sweet pastries;
- all types of fried foods;
- fatty meats and poultry (pork, lamb, duck);
- scrambled or hard-boiled eggs;
- sour berries;
- vegetables rich in coarse fiber (radish, raw onion, white cabbage, all pickled vegetables);
- fruits that contain a lot of carbohydrates (bananas, grapes);
- carbonated drinks and coffee.
The most common pancreatic diseases
The basics of this diet apply to most serious pancreatic diseases. But some disorders require special dietary habits. To understand which diet rules to follow, you need to learn to distinguish between pancreatic diseases.
Table 5. The most common pancreatic diseases
| Symptoms/Name of disease | Painful symptoms | Digestive system disorders | Features of the disease |
| Chronic pancreatitis | During exacerbation | In case of exacerbation or diet violation: constipation, loose stools, vomiting | Deterioration of health when departing from dietary rules |
| Cancerous formations | Depends on the location and size of the tumor | Irregular liquid diarrhea, vomiting | Pale skin with a possible yellowish tint, sudden weight loss |
| Tissue cyst | Depends on the location and size of the lesion, sometimes does not express itself | Depending on the location: diarrhea, bloating, vomiting, lack of stool, colorless stool | Manifest in the later stages in the form of acute pain and the possibility of palpation |
| Diabetes | Not expressed | Cloudiness with retching, vomiting, feeling of extreme hunger | Incessant thirst, scabies, dry mucous membranes, frequent urination, hypoglycemia |
The nutritional features of chronic pancreatitis are similar to the diet for acute pancreatitis - adherence to the principles described above, maintaining diet No. 5.
Pancreatic cancer
All products for pancreatic cancer must undergo preliminary heat treatment. You can only eat food at room temperature - too cold and hot foods irritate the affected area.
Preferable herbal teas without sugar that can soothe painful sensations: herbal tea, chamomile mint.
Sample menu for the day:
- Breakfast – low-fat kefir with a baked apple without sugar.
- Lunch – mashed buckwheat or rice with a slice of rye bread and a glass of juice.
- Lunch – steamed meat with stewed vegetables, a glass of jelly, a slice of bread.
- Snack – herbal infusion.
- Dinner – steamed omelette, chopped herbs, rosehip tea.
- Second dinner - a glass of skim milk.

Greens are a good substitute for spices that are prohibited for consumption by cancer patients
Pancreatic cancer is a serious cancer that can occur without any symptoms for a long time. How to recognize the first symptoms of this disease? Read more in our article.
Cyst
For the first 3 days after an exacerbation or surgery, you should not eat food in any form - only liquid. If the patient gets better, dietary foods can be gradually introduced into the diet.
Menu example:
- Breakfast - ground oatmeal of a liquid consistency with water or milk, herbal infusion.
- Lunch – low-fat homemade yogurt, biscuits, compote.
- Lunch – vegetable soup with boiled chicken or rabbit meat, buckwheat with steamed meat, fruit jelly.
- Snack – steamed omelette.
- Dinner – baked chicken fillet, cottage cheese casserole, weak tea.
- Second dinner - biscuits, low-fat kefir.
The diet for this disease is lightened - most flour products, beef, sour cream, semolina are allowed.
Diabetes
The main dietary restriction is the complete exclusion of confectionery, fried and fatty foods, and baked goods.
Daily diet:
- Breakfast – unsweetened cheesecakes, green tea, a slice of lemon.
- Lunch – grated oatmeal with water, dried fruits, compote.
- Lunch – lean borscht without beets, buckwheat with meat from a steamer, vegetable salad without dressing.
- Snack – a few slices of bread and juice.
- Dinner – stewed vegetables, steamed fish fillet, tea with milk.
- Second dinner - kefir.

The diabetic menu is as close as possible to classic healthy nutrition
Diet for the treatment of pancreatic disease
The secretory organ can become inflamed with the development of acute or chronic pancreatitis - this is one of the most common lesions, which has a different origin and can occur during a viral infection or with systematic alcoholization of the body.
A provoking factor in the occurrence of inflammation is an error in nutrition: abuse of too fatty, spicy, smoked foods, and alcoholic beverages.
When a gland disease has already occurred, it is important to understand that if you stick to the same diet before, the organ will simply stop working and serious consequences will occur in the body, including death.
Therefore, following a diet should become a habit and be strictly followed by all persons with such problems. Proper nutrition and diet for a sick stomach and pain in the pancreas is as necessary as air for life!
The basic principle of treating inflammatory processes in this organ is the following: “Cold, hunger and rest.” These methods were relevant many centuries ago, and they do not lose their significance to this day.
A patient with acute pancreatitis should be provided with complete rest and bed rest, apply cold to the diseased organ, and fast for several days.
In chronic forms outside of exacerbation, the tactics of therapeutic nutrition are not so strict and have their own characteristics that all patients must know. Violation of the diet, taking prohibited foods threatens the patient with exacerbation.
Reviews
Victoria: My son’s gland inflammation was accompanied by diarrhea. Pain haunted him constantly. We are being treated by a gastroenterologist. Only after following the diet did we achieve improvement. Moreover, by eating together, I lost seven kilos.
Anastasia: My problems with the pancreas arose recently. I lost weight dramatically, albeit temporarily, and the weight came back almost immediately. But this problem has been haunting me for two years now. I take pills all the time. I didn’t think about diet, I thought medications were the most important thing in treatment. I've been on a diet for 20 days now. The result is obvious. I began to feel better, even lost three extra pounds.
Marina: I have been suffering from pancreatitis for a long time, I am still obese, height 162 cm, weight 114 kg. No doctors could help until I went on a diet, table No. 5. At first it was hard, I always wanted fried foods and pickles. I got used to it from the second week. Of course, I had to forget about smoked, fried, salted and soda. After four weeks, I lost 8 kilograms.
Diet treatment for inflammation of the pancreas
The prescription of dietary recommendations by a doctor for inflammatory processes in the secretory organ follows the following principles:
- Suppression of enzyme activity and pancreatic juice;
- Reducing pain;
- Reducing body intoxication;
- Reducing the acidity of gastric juice;
- Providing functional rest to the organ;
- Normalization of liver and intestinal function;
- Stimulation of reparative processes of gland tissue;
- Fight against intoxication.
In the acute period of inflammatory changes in the organ with severe pain, high levels of enzymes in the blood, the patient is recommended to fast for 1-2 days, ingest alkaline mineral water of at least 1-1.5 liters, and weak tea at room temperature is allowed.
If, on the doctor’s recommendation, the fasting period needs to be extended for more than two days, patients are transferred to intravenous parenteral nutrition with solutions of amino acids, which are necessary for protein synthesis and maintaining the body’s energy balance.
If the exacerbation is not very pronounced and there is no need to prescribe the patient fasting, the doctor will prescribe the patient a gentle version of table No. 5p.
When inflammatory phenomena subside or in the remission phase, a less gentle, more physiological complete diet is recommended - an expanded version of table No. 5p.
I version of table No. 5p
A pancreatic sparing table is recommended for patients after several days of fasting in severe acute pancreatitis, or from the first days of a not very pronounced exacerbation of a chronic inflammatory process.
The duration of the first version of table No. 5p is up to seven days. This is a low-calorie, mechanically and chemically gentle diet for diseases of the pancreas, or when the stomach hurts.
The total caloric content should not exceed 1800-2000 kcal, the following content is allowed:
- Protein - 80 g
- Fat - 50 g
- Carbohydrates - 230 g
- Table salt - 6 g (in the absence of concomitant heart failure)
Food should be taken 5-6 times a day in small portions. Food should enter the stomach warm; it should not be too cold or hot.
The patient is allowed:
- Slimy cereal soups
- Vegetable puree
- Boiled river fish
- Steamed cutlets, meatballs, quenelles
- Meat soufflé
- Steamed egg white omelette
- Fresh low-fat cottage cheese
- Baked apples
- Grated buckwheat, boiled rice
- Dried fruit compotes
- Jelly
- Biscuits
- White bread
The patient is prohibited from:
- Raw vegetables (especially radishes, cabbage)
- High fiber fruits (legumes)
- Broths
- Coffee
- Sour juices
- Alcohol
- Kvass
- Soda
- Fast food
- Fatty fish and meat
- Spices
- Spices
- Canned food
- Pastries, cakes
- Mushrooms
All products that are difficult to digest and digest in the gastrointestinal tract, have a juice-like effect, contain extractive substances, cause increased gas formation and bloating should be strictly excluded from the diet.
Extended diet table No. 5
When general well-being improves, pain subsides, laboratory parameters normalize, and pancreatic inflammation goes into remission, a less sparing, more physiologically complete diet is prescribed.
It allows culinary processing of food in the oven, steaming. The energy value of the daily diet increases to 2500-2700 kcal, the amount of protein - 11 g, fat - 80 g, carbohydrates - 330 g, table salt - up to 8 g.
Like the previous option, the diet is dominated by proteins that the body needs to build its own cells and damaged tissues, replenish protein “hunger,” and accelerate recovery. Fats and carbohydrates are limited, especially those that are quickly absorbed - sweets, honey, jam.
This type of therapeutic nutrition is prescribed for a long time, and often it must be adhered to throughout life in order to avoid the development of repeated attacks and complications of pancreatitis.
The range of dishes and products allowed for consumption is approximately the same as in the list of acceptable consumption described above, with the difference that patients can also consume in moderate quantities:
- Lean meat not in pureed form, but in pieces
- Low-fat sour cream
- Soft-boiled egg
- Vegetable stew baked in the oven
- Raw mashed sweet apples
- Vegetable (10 g) or butter (8 g) oil, added to ready-made dishes
- Well-cooked porridge with milk
- Stale bread, biscuits
- Jelly
- Hard cheese varieties
Pancreatic disease: diet menu for the week
The menu is compiled on the recommendation of a doctor for a week, taking into account that 1 week of dietary nutrition includes the entire list of necessary products. The number of daily calories and meal times are taken into account.
As a rule, they create a menu for five meals a day. After 2 weeks, a correctly composed menu relieves inflammation of the gland and restores its normal activity. The patient feels significant relief, the disease recedes.
- First breakfast: boiled meat, pureed porridge, tea.
- Second breakfast: light omelet, boiled or baked fruit, a glass of herbal infusion.
- Lunch: vegetarian vegetable soup, steamed meat cutlets or meatballs with a side dish, sweet fruit jellies, jelly or compotes.
- Afternoon snack: a glass of tea with crackers.
- Dinner: fish or chicken soufflé, boiled vegetables.
- At night: kefir
In the first week, patients should adhere to approximately the following menu:
- Breakfast: oatmeal or buckwheat porridge; steamed meat cutlet; tea with milk.
- Second breakfast: low-fat cottage cheese; jelly.
- Lunch: vegetable soup; mashed potatoes; meat soufflé; apple compote.
- Afternoon snack: white bread crackers; rosehip decoction.
- Dinner: steam omelet made exclusively from proteins; semolina; tea.
- At night: 100 g of mineral water.
Features of menu planning in the second week of treatment:
- Breakfast : buckwheat or oatmeal porridge; lean boiled meat or steamed protein omelette; the vinaigrette.
- Second breakfast: dried fruits or pureed low-fat cottage cheese; cracker; weak tea or rosehip decoction.
- Lunch: vegetable or rice slimy soup; boiled or baked potatoes in foil; boiled chicken or boiled meat dumplings; fruit salad or jelly; apple.
- Afternoon snack : cottage cheese or baked apples; dried fruits compote.
- Dinner: pasta or carrot soufflé; boiled or steamed fish; tea.
- At night: a glass of kefir or rosehip decoction. Rose hip decoction is the best drink for a diseased pancreas.
Features of menu planning for chronic pancreatic diseases:
- Breakfast: milk oatmeal; boiled meat; tea. You can also prepare cheesecakes, rice, semolina, buckwheat porridge, mashed potatoes or carrots, boiled fish and meat, salads, and doctor’s sausage for breakfast.
- Second breakfast: steamed egg white omelette; rosehip decoction.
- Lunch: lean soup; boiled potatoes; beef stroganoff from lean boiled meat; dried fruits compote. You can diversify your lunch meal with cereal, fruit, milk soups, boiled chicken, veal, vegetables and cereals of any kind, jelly, fresh fruits and berries
- Afternoon snack: cottage cheese; tea with milk.
- Dinner: vegetable puree; boiled fish; tea. In addition, for dinner you can eat vegetable puree, omelettes, porridge from various cereals, and cottage cheese.
Diet menu for pancreatitis:
- Breakfast: (7:00-7:30): boiled beef, oatmeal with milk, tea.
- Second breakfast: (9:00–9:30) omelette, baked apple, rose hip decoction.
- Lunch: (12:00–13:00): vegetable soup, beef soufflé, pasta, sweet berry jelly, compote.
- Afternoon snack : (16:00–16:30): cottage cheese and tea.
- Dinner: (20:00–20:30): fish soufflé, tea.
Nutrition and diet after surgery to remove the pancreas
Surgical interventions to remove an important secretory organ or part of it can be performed for the following reasons: the development of complications of the inflammatory process with the formation of tissue death - pancreaticonecrosis, due to hemorrhages in the parenchyma of the gland, during oncological processes, peritonitis, cystic formations, abscesses, severe injuries with massive damage pancreas.
The body, left without part of an important glandular organ, or completely deprived of it, undergoes enormous stress and must have external support in the form of adequate medication, replacement therapy and lifelong diet.
In the early postoperative period, the patient is transferred to parenteral intravenous nutrition to reduce the load on the gastrointestinal tract.
A balanced composition of amino acids, broken down fatty acids, glucose is injected into the patient’s vein, nutrients enter the blood and are carried to organs and tissues, thereby supporting the body.
In the postoperative period, feeding through a tube with liquid semi-digested food can be performed. In the first postoperative week, caloric intake per day should not exceed 1000 kcal. You can drink water up to two times a day.
After seven days and the cessation of parenteral and tube nutrition, the patient is allowed to take food by mouth, but only in liquid and semi-liquid, mashed form.
This treatment is necessary for up to two months:
Liquid porridges, jelly, pureed vegetable soups are included in the list of permitted dishes. Calorie content at this recovery stage should not exceed 1900 kcal. The frequency of meals is 6-7 times a day, the volume of food eaten should not exceed the size of a fist.
After two months from the date of surgery, the diet gradually expands: dietary boiled meat, crackers, biscuits, low-fat cottage cheese and lactic acid products are introduced into it, and the consumption of bananas or baked apples is allowed.
The calorie content of food per day is 2000-2100 kcal. Meals are frequent, small, at least 6 times. The serving size is no larger than the palm of your hand.
During the recovery period, it is important to listen to your body, keep a food diary and carefully monitor the reaction of the gastrointestinal tract to the consumption of a particular product.
It is equally important, together with the diet, to carefully follow the doctor’s medication prescriptions and take prescribed enzyme and replacement drugs that normalize digestion and perform the functions of a remote organ exactly on schedule.
If a patient after a pancreatic surgery experiences discomfort in the abdomen after eating, vomiting, diarrhea or nausea, or other manifestations of dyspepsia, you should definitely consult a doctor.
The pancreas is an important regulator of the processes of the digestive canal. It is assigned a number of vital functions, so any violations in its activities require immediate action. One of the most effective is a diet for pancreatic disease.

Nutrition after surgery
If surgery is performed, resection of part or all of the pancreas, diet becomes vital. The patient must fast for several days after the operation. You are only allowed to drink one liter of still mineral water per day.
Based on the patient’s condition, the doctor prescribes dishes, first light steam omelettes. Buckwheat or rice porridges are gradually allowed. After 6–7 days, include meat dishes, fish soufflés, meatballs and steamed cutlets.
After discharge, the patient needs to organize appropriate conditions so that he can eat food after 2-3 hours, always freshly prepared.
In addition, a person after pancreatic resection should not expose himself to serious tests and stress.
Pathologies of the pancreas, general information
Symptoms of the disease will help you recognize the presence of pancreatic pathology. First of all, the disease is indicated by pain localized in the upper zone of the abdominal cavity. The pain syndrome can appear constantly or have a certain periodicity. The occurrence of discomfort is associated with the increased activity of the enzymatic components of this organ, which attack their own cells.
Pathological conditions of the pancreas are in close relationship with lesions of other organs of the digestive tract, liver and bile ducts. The most common pancreatic disease is pancreatitis.
With any damage to this organ, changes occur in its functioning. There is a disruption in the outflow of pancreatic juice, which enters the digestive canal. The result of this phenomenon is a disruption of digestive processes that do not proceed properly. Therefore, the body suffers from a lack of necessary components.
To alleviate the patient's condition, he is prescribed medications. However, if you do not adhere to the necessary therapy and do not follow a strict diet, the disease can become chronic, and over time even cause more serious changes, such as malignant neoplasms.
When the disease is in a state of exacerbation, it is recommended to completely abandon any food, because it is when it is taken that active production of enzymes occurs. As a rule, the occurrence of pain is accompanied by loss of appetite.
For patients suffering from pancreatitis or other pancreatic pathologies, a special strict diet No. 5 is prescribed. The main goal of such a measure is to reduce the load on the affected organ, correct impaired metabolic processes and supply the body with missing micronutrients.
General nutrition rules

According to the observations of specialists, if you follow all the nutritional rules, the stage of exacerbation of pancreatic pathologies can be alleviated.
If there are no symptoms of the disease, then the daily menu should be divided into 5 meals a day. All foods that contribute to the development of constipation or bloating should be excluded.
Useful foods for pancreatic diseases

In order for the benefits of the diet to be maximum, it must be enriched with protein and those foods that cannot lead to fat and vitamin deposition.
Excess fat should be avoided, but it is advisable to give preference to protein foods.
Nutritionists recommend replenishing the necessary reserves of carbohydrates by consuming honey, jam, fruits, and vegetables.
The patient's daily diet may contain the following foods and dishes:
- low-fat dairy products
- chicken or turkey without skin
- rabbit, lean beef
- boiled vegetables
- vegetarian soups with grated vegetables and boiled cereals
- rice, oatmeal, buckwheat and semolina porridges should have a viscous consistency
- soft ripe fruits and berries are allowed
- It is possible to flavor ready-made dishes with vegetable or butter.
What dishes can be presented on the menu for lesions of the pancreas and liver:
- cottage cheese with milk
- cheesecakes, only low-fat ones
- buckwheat or rice porridge
- cabbage cutlets
- boiled fish
- dishes prepared from lean meat.
- milk noodle soup
- cereal porridge with boiled chicken
- vegetables
- berry jelly
- vegetable stew
- potatoes with boiled fish
- porridge without adding oil
- kefir
- Before going to bed, you are allowed to eat dried apricots or prunes.
If pancreatic pathology develops in children and adults, it is necessary to fast for two days and drink liquids only with the doctor’s permission. Only from the third day cottage cheese, vegetable puree, and liquid porridge are added to the diet. This diet must be followed for at least 7 days.
As the patient's exacerbation period passes, he is gradually transferred to a special diet.
The selection of dietary intake and nutritional adjustments for patients with pathologies affecting the pancreas should be carried out exclusively by a specialist.
Prohibited Products
With the development of any diseases of the pancreas, it is necessary to ensure the mandatory exclusion of products containing essential oils, acids, as well as substances that can activate increased production of pancreatic juice.
Fried, salty, spicy, pickled, and fatty foods are strictly contraindicated.
It is necessary to remove from the diet:
- the presence of fatty meat and fish broths, okroshka, mushroom soup, sour cabbage soup;
- fatty types of meat, fish, offal;
- smoked sausage;
- caviar, pates, canned food, lard;
- fried or hard-boiled eggs;
- fresh bread, baked goods;
- various seasonings, spices, horseradish, mustard;
- onions, garlic, rhubarb, sorrel, mushrooms;
- chocolate products, coffee, cocoa, confectionery;
- any alcoholic products.
Only by eliminating all of the listed products from consumption can you count on a speedy recovery.

Recipes for healthy dishes for pancreatic diseases
Finding yourself face to face with an unpleasant illness, first of all you will have to limit yourself to many products. But even from that small list of permitted ones, you can prepare a variety of delicious delicacies. Here are the recipes for some of them.
To prepare such a soup, you cannot do without zucchini, broccoli, cauliflower, and sweet peppers. Well-washed vegetables are cut into small cubes. Place them in a saucepan, add 1.5 liters of water and boil until ready. Before use, the liquid is drained, and the cooked vegetables must be ground in a blender until pureed.
- Steamed fish
The fish fillet is washed, placed on a steamer and simmered for 15 minutes. Before use, lightly add salt, you can flavor it with a little butter.
The peeled pumpkin is washed, cut into cubes, placed in water and cooked over medium heat for about 20 minutes. Then the liquid is drained and the pumpkin is mashed with a fork or chopped with a blender. It is allowed to add a small amount of butter, sugar or honey to the porridge.
Place chicken meat in water and let it boil. After this, the liquid is drained and vegetables are added to the chicken meat. Everything is filled with water and boiled until the chicken is ready. Mashed potatoes or porridge are suitable as a side dish for this dish.
Important! When dieting, consistency is important. You should train yourself to have meals at the same hours.
The nutritional regimen for the development of pancreatic pathologies should be developed individually for each specific case. If you strictly follow all the prescribed nutritional rules, the patient will be able to minimize painful attacks. Diet alone without the use of medications cannot cure a patient. But even without a well-designed diet, it will also not be possible to achieve the desired result.

Work experience more than 7 years.
Professional skills: diagnosis and treatment of diseases of the gastrointestinal tract and biliary system.










