A proper diet for pancreatitis and gastritis is the key to success in treating the disease. Organizing proper nutrition is not difficult. To do this, you need to know which products are allowed and which are not. It is also important to remember the advice of nutritionists regarding diet and instructions for preparing certain dietary dishes.
What is pancreatitis
Pancreatitis is an acute or chronic inflammation of one of the main organs of the endocrine system of our body - the pancreas.
The functioning of the entire gastrointestinal tract and the process of food digestion depend on the normal functioning of this organ. The pancreas is located in close proximity to the liver, right behind the stomach. It performs many functions, the main one of which is the synthesis of hormones, in particular insulin. It also produces digestive enzymes that ensure the breakdown and absorption of fats, proteins and carbohydrates. Digestion of food occurs under the influence of pancreatic juice, which enters directly into the duodenum.
Enzymes and pancreatic juice begin to be produced immediately after any food or drink enters the stomach. Enzymes perform different tasks:
- lipase - breaks down fats;
- lactase, amylase, maltase and invertase convert carbohydrates into monosaccharides - glucose, galactose and fructose;
- trypsin - ensures the body's absorption of proteins.
In essence, pancreatitis is self-poisoning of pancreatic tissue by the enzymes it produces. Inflammation begins with excessive production of certain enzymes in combination with increased pressure in the ducts of the gland. Excess enzymes enter the general bloodstream, negatively affecting the functioning of the brain, kidneys and other internal organs.
Causes of inflammation of the pancreas:
- Alcohol abuse. More than half of the observations (p. 36-47) of pancreatitis are associated with regular consumption of large doses of alcohol.
- Pancreatitis often develops with cholelithiasis, abdominal trauma, the formation of cysts in the bile ducts, and malignant tumors in the gland.
- The disease can be a side effect of taking certain medications, such as diuretics.
The risk group includes diabetics, people with other endocrine pathologies and hepatitis B or C. Sometimes pancreatitis develops during pregnancy or after a kidney transplant.
How does alcohol affect the functioning of the pancreas?
Alcohol breaks down in the body to form acetaldehydes, which are toxic to humans. Pancreatic cells are especially susceptible to their harmful effects. In addition, drinking alcohol can cause spasms and narrowing of the pancreatic ducts, which leads to the accumulation of pancreatic juice in it. As a result, digestive enzymes begin to process the gland itself, causing inflammation. Over time, if the disease is not treated, the cells of the gland die (pancreatic necrosis) and are replaced by scar tissue, the organ loses the ability to function as before.
It is important to understand that the type of drink and its quality do not matter in this case. If a drink contains alcohol, it is harmful. Drinking alcohol together with fatty foods or foods with a high glycemic index can have a particularly negative effect on the functioning of the pancreas, since these products create additional stress on the organ.
Table 5p
Diet number 5p is a classic table for pancreatitis. The letter “p” attached indicates the type of nutrition of the Pevsner classification. A balanced diet was specially developed to improve the functioning of the pancreas.
In diet number 5p, fats in permitted foods are strictly calculated. The main meal consists of:
- slimy cereal soups;
- pureed vegetable stew;
- salads of boiled beets and carrots;
- baked apples without peel;
- steamed egg white omelettes;
- steam cutlets from twice ground chicken or turkey fillet.
To compensate for the necessary fats, oils are gradually added to dishes: olive, flaxseed.
Types of pancreatitis
The most general classification of pancreatitis is based on the nature of the disease: acute attack or prolonged chronic pancreatitis with periodic relapses. The two forms differ in the severity of symptoms and require different treatment approaches.
Acute pancreatitis
The inflammatory process in acute pancreatitis develops very quickly and is always accompanied by severe pain. In most cases, the disease occurs due to alcohol abuse or after eating large amounts of fatty foods. Sometimes an exacerbation is preceded by an attack of acute hepatic colic.
Symptoms of acute pancreatitis:
- Severe pain in the left hypochondrium, radiating to other organs. The painful attack lasts about half an hour to an hour. The pain is felt especially strongly when lying on your back. The attack intensifies after eating food, especially fried and spicy food, and any alcoholic beverages.
- Vomiting, often uncontrollable with an admixture of bile and a bitter taste. Constant nausea that does not go away after vomiting.
- Low-grade or high fever.
- Sometimes, due to a violation of the outflow of bile, yellowing of the eye whites is observed, very rarely - a yellow tint to the skin.
- In some cases, the pain syndrome is accompanied by heartburn and bloating.
An attack of acute pancreatitis requires immediate medical attention. Painkillers provide only temporary relief, but do not affect the cause of inflammation. In the absence of qualified assistance, the risk of severe complications quickly increases: infection in inflamed tissue, necrosis and abscesses.
Severe acute pancreatitis can lead to shock and multiple organ failure.
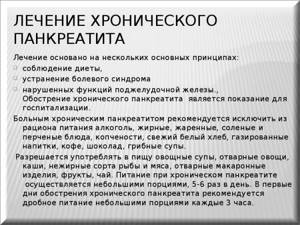
Chronic pancreatitis
If, after an attack of acute pancreatitis, a person does not follow doctors’ recommendations and continues to drink alcohol and eat poorly, the disease is highly likely to enter the chronic stage. Chronic pancreatitis develops when there is significant damage to the pancreas during the first episode of the disease.
The disease is characterized by gradual pathological changes in the structure of pancreatic cells. Over time, it begins to lose its main function - the production of enzymes necessary for digesting food. Exocrine insufficiency manifests itself:
- diarrhea,
- bloating,
- a change in the nature of feces - they acquire a sticky consistency due to the large amount of fat in them and are poorly washed off the walls of the toilet.
Chronic pancreatitis can be asymptomatic for a long time: acute pain appears when significant pathological changes have already occurred in the pancreas. During an attack, chronic pancreatitis manifests itself with the same symptoms as acute:
- severe girdle pain,
- nausea,
- vomit,
- disturbances in intestinal function.
The diagnosis is made on the basis of ultrasound, computed tomography or magnetic resonance imaging. The examination usually reveals narrowed pancreatic ducts due to the formation of stones in them - calcifications. Hardware techniques also make it possible to detect cysts in place of atrophied tissue. Laboratory blood tests for chronic pancreatitis are not very informative.
Pancreatic insufficiency is determined by analyzing stool. If they contain a specific enzyme, pancreatic elastase, a diagnosis of chronic pancreatitis is made.
Dish recipes
Food can be not only useful in the treatment of gastritis and pancreatitis, but also tasty if you know how to prepare it correctly. Below are the most popular recipes that will help diversify your diet menu and enjoy the taste of the products.
Meatballs with carrots
Small carrots are peeled, grated on a fine grater and placed on the bottom of an enamel bowl. Fill with water and put on fire.
For minced meat, you can use boneless chicken or turkey fillet (sometimes lean veal is allowed). Grind twice in a meat grinder, achieving maximum grinding. Finely chopped herbs (green parsley is best) and a small pinch of salt are added to the minced meat. Roll the mixture into small balls with a tablespoon and lower them one by one into boiling water (this will prevent them from falling apart).
The meatballs are cooked for 20–25 minutes and then removed from the water. The water is drained through a colander, and the boiled carrots are used as a side dish.
Thanks to thorough mashing, the meat will be easily digestible, and because of the carrots, it will seem juicy and very tasty. Vegetable puree soup
Usually such a soup is prepared with a second chicken broth, but it will be delicious without it.
Pour peeled and diced vegetables into boiling broth or just water (the liquid should barely cover the vegetables).
Combinations of:
- carrots and zucchini;
- potatoes with eggplants;
- pumpkins with carrots;
- potatoes with beets and celery.
Vegetables are cooked until fully cooked (when checking, the cube can be easily cut in water with a knife). Part of the water is poured into a mug to make it easier to crush the vegetables to a homogeneous consistency.

Add chopped herbs (fresh dill or parsley) to the cooked vegetables, lightly add salt and pound, gradually adding vegetable broth from the mug.
Before serving, you can add some crackers to the puree soup. You can sprinkle the dish with a handful of flax seeds or sesame seeds - these healthy additives, rich in valuable elements, are an alternative to bread.
Importance of enzymes in digestion
The functioning of the human body is ensured by a complex system of interconnected and interdependent biochemical reactions. Thanks to special protein compounds - enzymes or enzymes - all these reactions are accelerated, ensuring rapid metabolism. The action of enzymes is very selective: each of them is capable of initiating, accelerating or slowing down only one reaction.
The digestive process is based on the work of digestive enzymes. Their main task is to make the process of energy absorption fast and efficient. Enzymes break down food components (proteins, fats and carbohydrates) into substances suitable for absorption. Moreover, the amount of enzymes produced depends on the quantity and quality of what is eaten.
Digestion of food begins in the oral cavity. The food, crushed into small pieces by the teeth, is mixed with saliva, which contains the enzyme alpha-amylase. The better we chew food, the easier it is for the enzyme in the salivary glands to convert starch molecules into soluble sugars and facilitate further processing.
After initial processing, food enters the stomach through the esophagus, where the gastric enzyme pepsin and hydrochloric acid begin to work. These substances create gastric juice, which:
- provides antibacterial protection for the body;
- stimulates the production of pancreatic hormones;
- regulates gastric motility;
- breaks down fats and performs a number of other functions.
In addition to pepsin, which is responsible for the breakdown of large protein molecules, other enzymes are produced in the stomach, for example:
- gelatinase is a solvent for collagen, gelatin and other connective tissue proteins;
- lipase is an enzyme that breaks down some fat molecules into fatty acids and monoglycerides;
- chymosin - starts the process of digesting milk protein.
Bile plays a significant role in the digestion process. It contains bile acids that stimulate the production of pancreatic secretions.
From the stomach, the food bolus is evacuated into the duodenum, where the main process of food digestion occurs. It is provided by more than 20 pancreatic enzymes. Enzymes are contained in pancreatic juice, which is produced by the gland in a volume of about two liters per day.
Functions of pancreatic enzymes:
- proteases - breakdown of proteins into amino acids;
- nucleases - act on DNA nucleic acids;
- amylase - breaks down starch into simple sugars;
- lipases - break down fats into higher fatty acids and glycerol.
The digestion process is completed under the action of enzymes of the small intestine and beneficial bacteria living in the intestines. The intestines absorb processed food into the body (Fig. 1).

Figure 1. Some important digestive enzymes. Source: Jason Northwest
When the function of enzyme production by the organs of the digestive system, especially the pancreas, is disrupted, the entire body becomes unbalanced. Such an imbalance entails nausea, diarrhea, flatulence, followed by anemia and exhaustion.
What to take with meals if you have a deficiency of pancreatic enzymes
With pancreatitis, the process of production of digestive enzymes by the pancreas is disrupted, as a result of which a person suffers from discomfort and pain in the stomach. In this case, after a complete examination, replacement therapy may be prescribed.
The goal of treatment with enzyme preparations is to compensate for their deficiency in the body, while reducing the load on the damaged organ. In some cases, such therapy is prescribed for life.
Important! The effect of all enzyme preparations begins 20-30 minutes after eating, so you need to drink them strictly before meals in the dosage prescribed by your doctor!
Modern pharmacology offers a large number of different enzyme preparations of animal and plant origin. Some of them are aimed only at replenishing the deficiency of a single enzyme, for example, one that breaks down lactose or fats. There are also complex agents prescribed for the deficiency of several enzymes in various organs of the digestive system.
Pancreatic enzymes are obtained from the organs of cows or pigs. The composition of the medicines includes the main pancreatic enzymes - amylase, lipase and trypsin. Polyenzyme preparations, in addition to pure pancreatin, may include bile acids, adsorbents or other enzymes. All drugs are selected strictly individually, taking into account the nature of the disease and the severity of symptoms.
Finally
what to eat during exacerbation of pancreatitis
The 7 day menu is approximately the same as the 6 day menu. Meals should be taken in a calm environment. You can't rush or stand while eating. You need to chew your food very carefully. Compote, tea, decoctions must be warm. Drinking cold water is prohibited.
Pancreatitis is a chronic acute disease characterized by an inflammatory process in the pancreas. During this process, the internal tissues of the pancreas are significantly damaged, up to their complete collapse. As a course of treatment, medical experts recommend undergoing a special diet.
Why do you need a diet for pancreatitis?
In the treatment of pancreatitis, nutrition plays no less a role than medications. The main goal of the prescribed diet is to restore the functions of the pancreas and normalize the production of digestive enzymes.
Products that are difficult to process increase the load on the inflamed organ. After a rich feast with fatty fried foods, the pancreas begins to intensively produce enzymes for its digestion. If the ducts of the gland are narrowed, pancreatic juice produced in extreme mode accumulates in the gland, aggravating the development of the disease - the affected pancreas begins to digest itself.
Signals that the gland is working overtime include:
- heaviness in the stomach after eating,
- heartburn,
- burping,
- attacks of pain in the stomach.
Of course, sticking to a strict diet all the time is not easy, especially at home. People with strict dietary restrictions are forced to cook for themselves separately and resist the temptation to eat anything fried or spicy.
It is important to understand that one violation of the diet can cause an acute attack of pancreatitis with all the ensuing consequences: severe pain, nausea, vomiting and diarrhea. A single failure can negate all efforts to maintain long-term remission.
General tips for organizing meals
The main thing in diet therapy is a clear distinction between foods that are beneficial and those that are harmful. There are a number of products that can be found on the approved lists. But even they become dangerous if used incorrectly.
For example, if you have pancreatitis or gastritis, it is acceptable to eat steamed egg omelet. But hard-boiled eggs are strictly prohibited by gastroenterologists. Baked chicken meat is a provocateur of exacerbation of pancreatitis or gastritis. While chicken broth has a healing effect on the inflamed organs of the gastrointestinal tract.

If we talk about cooking methods, we definitely exclude frying, smoking and drying. Products for the diet menu are boiled or cooked until ready by steaming, in a slow cooker, or in the oven.
Authorized Products
During periods when pancreatitis and gastritis are exacerbated, ingredients that do not increase the acidity of the stomach and do not irritate the mucous membrane are considered the least dangerous.
Table of allowed food groups:
| Flour products | Yesterday's bread (preference – whole grain, rye, wheat), homemade crackers, dryers, biscuits, crispbread. During periods of remission - noodles and spaghetti (up to 170 grams per serving). |
| Cereals | Rice, buckwheat, oatmeal, semolina. |
| Types of vegetables and herbs | Vegetables include potatoes, pumpkin, beets, carrots, eggplants, and zucchini. You can add 1 tbsp daily. l. chopped celery, parsley and dill. |
| Fish dishes | You can eat the pulp of varieties with the lowest fat content (hake, cod, pike perch), boiled or cooked in a slow cooker. Fish meatballs and broths. |
| Seafood | Sea kale. |
| Meat menu | For preparing broths, steamed cutlets and meatballs, preference is given to chicken, rabbit, turkey, and lean veal. |
| Fermented milk | Kefir, low-fat cottage cheese, cheese are not prohibited with normal or low stomach acidity. |
| Eggs | Steamed omelette made from chicken and quail eggs. |
| Oil | Refined sunflower, olive, flaxseed, pumpkin. In stable remission - creamy (no more than 30 grams per day). |
| Fruits | Bananas, baked apples. |
| Bee products | Honey, propolis, royal jelly. |
| Spices | Sesame, fennel, cumin, turmeric, cloves. |
Decoctions of herbs or rose hips, Borjomi, weak black tea, and homemade jelly are recommended for drinking.
Note: the described ingredients constitute a special menu number 5 in its expanded form, intended for people with pancreatitis, gastritis, cholecystitis and hepatitis.
Prohibited Products
In fact, all components that are not included in the table approved by gastroenterologists are considered harmful to people suffering from pancreatitis and gastritis. This means that “taboo” is declared:
- any smoked meats;
- preserves and marinades;
- spicy and sour dishes;
- fatty varieties of fish, meat, cheeses;
- mushrooms;
- sweet and rich baked goods;
- nuts and seeds;
- coffee, alcohol, carbonated drinks.

Legumes (peas, beans, corn) are prohibited - they cause bloating and belching. Regular cabbage is dangerous - its acid provokes heartburn. The same applies to sorrel, spinach, radish, and lettuce. A categorical “no” will have to be said to horseradish, garlic and onions, including green ones.
During the remission stage, a small amount of salt is allowed. Iodized is best. It is recommended to add salt to dishes at the end of cooking.
What herbs can you drink?
To alleviate the condition, after consulting a doctor, you can drink decoctions of medicinal herbs.
Yelan
“Elan” is a ready-made collection of Altai herbs, sold in pharmacies. Has an anti-inflammatory effect. The decoction should be prepared according to the recommendations on the package.
Parsley
Parsley has a pronounced anti-inflammatory and antioxidant effect, stimulates gastric secretion. For chronic pancreatitis, an infusion of fresh chopped parsley is taken 2-3 times a day, half an hour before meals.
Herbal mixture No. 213
The collection includes a number of plants useful for inflammation: chamomile, wormwood, horsetail and other herbs. Decoctions based on the collection are prepared according to the recommendations on the packaging.
Fully or partially limited products
- Rye and fresh wheat bread, cakes, pastries with cream, puff pastry, baked goods, yeast pies.
- Soups with meat, mushroom, and fish broths, borscht and cabbage soup, cold soups (okroshka, beetroot soup).
- All fried foods, fried pies, cheesecakes, pancakes and pancakes.
- Fatty meat and fish (sturgeon, salmon, halibut), goose and duck meat, smoked meats, caviar, salted fish, sausages, canned food, fried and stewed fish. Organ meats (liver, kidneys, brains), as they contain a lot of cholesterol .
- Crumbly porridges (limit or completely exclude pearl barley, millet, corn, barley).
- Vegetables with coarse fiber (radish, turnip, rutabaga, white cabbage, eggplant), legumes, mushrooms in any form. The exception is soybeans.
- Raw vegetables and fruits are introduced very carefully. At the initial stage of the diet, they are recommended only in boiled or baked form.
- Cooking fats and lard (pork, beef and lamb) are excluded.
- Fruits containing large amounts of simple carbohydrates (bananas, grapes, dates), which can cause bloating.
- Milk soups.
- You should not eat hard-boiled or fried eggs, full-fat milk, cream, fatty sour cottage cheese, or salty, spicy cheese.
- Hot seasonings and spices: horseradish, herbs, mustard, pepper, ketchup, mayonnaise.
- Black coffee, chocolate, ice cream, cocoa, grape juice, alcoholic and carbonated drinks are also excluded.

Vegetables prohibited for pancreatitis
Table of prohibited products
| Proteins, g | Fats, g | Carbohydrates, g | Calories, kcal | |
Vegetables and greens | ||||
| canned vegetables | 1,5 | 0,2 | 5,5 | 30 |
| eggplant | 1,2 | 0,1 | 4,5 | 24 |
| swede | 1,2 | 0,1 | 7,7 | 37 |
| peas | 6,0 | 0,0 | 9,0 | 60 |
| cabbage | 1,8 | 0,1 | 4,7 | 27 |
| bulb onions | 1,4 | 0,0 | 10,4 | 41 |
| chickpeas | 19,0 | 6,0 | 61,0 | 364 |
| salad pepper | 1,3 | 0,0 | 5,3 | 27 |
| parsley | 3,7 | 0,4 | 7,6 | 47 |
| radish | 1,2 | 0,1 | 3,4 | 19 |
| white radish | 1,4 | 0,0 | 4,1 | 21 |
| dill | 2,5 | 0,5 | 6,3 | 38 |
| beans | 7,8 | 0,5 | 21,5 | 123 |
| horseradish | 3,2 | 0,4 | 10,5 | 56 |
| spinach | 2,9 | 0,3 | 2,0 | 22 |
| sorrel | 1,5 | 0,3 | 2,9 | 19 |
Fruits | ||||
| bananas | 1,5 | 0,2 | 21,8 | 95 |
Berries | ||||
| grape | 0,6 | 0,2 | 16,8 | 65 |
Mushrooms | ||||
| mushrooms | 3,5 | 2,0 | 2,5 | 30 |
| marinated mushrooms | 2,2 | 0,4 | 0,0 | 20 |
Nuts and dried fruits | ||||
| nuts | 15,0 | 40,0 | 20,0 | 500 |
| raisin | 2,9 | 0,6 | 66,0 | 264 |
| seeds | 22,6 | 49,4 | 4,1 | 567 |
| dates | 2,5 | 0,5 | 69,2 | 274 |
Cereals and porridges | ||||
| corn grits | 8,3 | 1,2 | 75,0 | 337 |
| millet cereal | 11,5 | 3,3 | 69,3 | 348 |
| barley grits | 10,4 | 1,3 | 66,3 | 324 |
Flour and pasta | ||||
| pasta | 10,4 | 1,1 | 69,7 | 337 |
| dumplings | 11,9 | 12,4 | 29,0 | 275 |
Bakery products | ||||
| buns | 7,9 | 9,4 | 55,5 | 339 |
| Rye bread | 6,6 | 1,2 | 34,2 | 165 |
Confectionery | ||||
| pastry cream | 0,2 | 26,0 | 16,5 | 300 |
| shortbread dough | 6,5 | 21,6 | 49,9 | 403 |
Ice cream | ||||
| ice cream | 3,7 | 6,9 | 22,1 | 189 |
Chocolate | ||||
| chocolate | 5,4 | 35,3 | 56,5 | 544 |
Raw materials and seasonings | ||||
| mustard | 5,7 | 6,4 | 22,0 | 162 |
| mayonnaise | 2,4 | 67,0 | 3,9 | 627 |
Dairy | ||||
| milk 4.5% | 3,1 | 4,5 | 4,7 | 72 |
| cream 35% (fat) | 2,5 | 35,0 | 3,0 | 337 |
| whipped cream | 3,2 | 22,2 | 12,5 | 257 |
| sour cream 30% | 2,4 | 30,0 | 3,1 | 294 |
Cheeses and cottage cheese | ||||
| parmesan cheese | 33,0 | 28,0 | 0,0 | 392 |
Meat products | ||||
| fatty pork | 11,4 | 49,3 | 0,0 | 489 |
| salo | 2,4 | 89,0 | 0,0 | 797 |
| bacon | 23,0 | 45,0 | 0,0 | 500 |
Sausages | ||||
| smoked sausage | 9,9 | 63,2 | 0,3 | 608 |
Bird | ||||
| smoked chicken | 27,5 | 8,2 | 0,0 | 184 |
| duck | 16,5 | 61,2 | 0,0 | 346 |
| smoked duck | 19,0 | 28,4 | 0,0 | 337 |
| goose | 16,1 | 33,3 | 0,0 | 364 |
Fish and seafood | ||||
| smoked fish | 26,8 | 9,9 | 0,0 | 196 |
| black caviar | 28,0 | 9,7 | 0,0 | 203 |
| salmon caviar granular | 32,0 | 15,0 | 0,0 | 263 |
| salmon | 19,8 | 6,3 | 0,0 | 142 |
| canned fish | 17,5 | 2,0 | 0,0 | 88 |
| salmon | 21,6 | 6,0 | — | 140 |
| trout | 19,2 | 2,1 | — | 97 |
Oils and fats | ||||
| animal fat | 0,0 | 99,7 | 0,0 | 897 |
| cooking fat | 0,0 | 99,7 | 0,0 | 897 |
Alcoholic drinks | ||||
| dry red wine | 0,2 | 0,0 | 0,3 | 68 |
| vodka | 0,0 | 0,0 | 0,1 | 235 |
| beer | 0,3 | 0,0 | 4,6 | 42 |
Non-alcoholic drinks | ||||
| soda water | 0,0 | 0,0 | 0,0 | — |
| cola | 0,0 | 0,0 | 10,4 | 42 |
| instant coffee dry | 15,0 | 3,5 | 0,0 | 94 |
| sprite | 0,1 | 0,0 | 7,0 | 29 |
Juices and compotes | ||||
| grape juice | 0,3 | 0,0 | 14,0 | 54 |
| * data is per 100 g of product | ||||
Diet for pregnant women
Pregnant women often face problems related to the functioning of the gastrointestinal tract. Pancreatitis can develop due to abuse of vitamin complexes or due to excessive pressure on the pancreas from the uterus.
The principles of the diet for pregnant women do not differ from the general diet for pancreatitis. However, during pregnancy it is extremely important to provide a nutritious diet necessary for the development of the fetus. The following must be present in the food in sufficient quantities:
- proteins (lean meat and fish, dairy products, eggs, legumes),
- complex carbohydrates (cereals, pasta, fruits and vegetables),
- fats (vegetable oils),
- vitamins and minerals.
Sample menu for the week (for every day), what can you eat and what should the food be?
Nutritionists have developed ready-made approximate meal plans for patients with gastritis and pancreatitis. This greatly simplifies the task of organizing proper nutrition at home.
The table shows one of the most common weekly menu options:
| Day of the week | Name of meal | Dishes and products |
| Monday | Breakfast | Semolina porridge cooked in water. |
| A piece of yesterday's bread with honey. | ||
| Tea. | ||
| Light snack | Vegetable salad. | |
| Still water. | ||
| Dinner | Chicken broth with rice noodles. | |
| Meatballs made from rabbit or turkey meat with vegetables. | ||
| Berry juice or jelly. | ||
| Afternoon snack | A glass of kefir. | |
| Dinner | Cottage cheese casserole cooked in a slow cooker. | |
| Plantain decoction. | ||
| Tuesday | Breakfast | Steamed egg omelette. |
| Light snack | Baked apple with honey. | |
| Dinner | Zucchini puree soup. | |
| Afternoon snack | A glass of jelly. | |
| Dinner | Fish and potato casserole. | |
| Wednesday | Breakfast | Cheese pancakes from a multicooker. |
| Light snack | Kefir with biscuits. | |
| Dinner | Carrot puree soup with black breadcrumbs. | |
| Afternoon snack | Berry jelly. | |
| Dinner | Pumpkin puree. | |
| Thursday | Breakfast | 1 soft-boiled egg. |
| Light snack | Rosehip decoction with honey. | |
| Dinner | Potato and carrot soup with low fat cheese. | |
| Afternoon snack | Baked apple. | |
| Dinner | Steamed fish cutlets. | |
| Friday | Breakfast | Rice cooked in water. |
| Light snack | Baked apple with honey. | |
| Dinner | Chicken soup with breadcrumbs. | |
| Afternoon snack | Oatmeal jelly. | |
| Dinner | Buckwheat porridge with flaxseed oil. | |
| Saturday | Breakfast | Oatmeal with water. |
| Light snack | Banana with honey. | |
| Dinner | Turkey meatball soup. | |
| Afternoon snack | Plantain decoction with dried fruits. | |
| Dinner | Boiled fish. | |
| Sunday | Breakfast | Semolina. |
| Light snack | Kefir with biscuits. | |
| Dinner | Rice soup with pieces of white meat chicken. | |
| Afternoon snack | 2 baked apples. | |
| Dinner | Stewed zucchini. |
Dishes can be alternated in a circle. Or rearrange for next week. It is advisable to ensure that variety is maintained: if you already had oatmeal for breakfast, then it is better to postpone the oat jelly to the next day.
Reviews and results
Nutritional therapy loses its meaning if it is not strictly followed and if the patient is not convinced of the need for it. This dietary table is complete in protein content and can be followed by patients for a long time. Reviews note rapid relief: pain and bloating are eliminated, stools are normalized. Many note that they are forced to constantly adhere to dietary nutrition due to their health status, since expanding the diet causes deterioration. The reviews also indicate certain difficulties: individual cooking requires knowledge of the technology of its preparation and time.
- “... I was admitted to the hospital with acute pancreatitis. They found gallstones and said that they were the cause of pancreatitis. The condition was not very serious, but I still spent 3 weeks in the hospital (surgery and then gastroenterology). Therefore, I know the diet very well - I went through all its options. After discharge, I continue to do it, they said 6 months and described approximately what products and how to introduce them when expanding the diet. I do everything very strictly, because I am afraid of exacerbation. I don’t want to have surgery - I’d rather eat right. I feel good: there is no pain or bitterness, my stomach is not swollen, and food is digested well. Of course, it’s difficult to do it - I’m tired of steamed, ground and almost tasteless food, which is not familiar to a healthy person. But with my illnesses, I have nowhere to go”;
- “... With chronic pancreatitis, I strictly monitor my nutrition and follow the basic diet constantly (almost all foods can and do not need to be ground, but this is good). But even from the approved products, I don’t tolerate everything well. For example, pearl barley and millet porridge are difficult for me - immediately bloating and pain in the intestines (probably also colitis). After so many years, I have already adapted to preparing the necessary dishes. At first a simple double boiler helped, but now I bought a multicooker - it helps a lot and you can cook much more dishes in it. I teach the whole family to eat properly”;
- “... I have chronic cholecystitis and pancreatitis. Diet number 5 is the main one for me and I studied it very well. Once a year I am treated in a hospital (usually an exacerbation in the spring), and the rest of the time I only eat diet food and take enzymes periodically. Only this allows you to feel good (without pain and heaviness under the ribs). Over the course of her long history of illness, she adapted to quickly making steamed dishes and soufflés. Of course, I don’t have the opportunity to cook every day, so I make cutlets and quenelles for 2-3 days, and then steam them. When there is no exacerbation, nutrition is complete and healthy (without fried, spicy and fatty foods). My family supports me."
Consequences
Failure to comply with the diet threatens the patient with serious consequences. As complications of pancreatitis, diseases such as:
- Hypertension (hepatic);
- Diabetes mellitus of the first or second type;
- Jaundice;
- Any gastrointestinal diseases;
- Pancreatic cancer;
- Brain damage.